Viruses that have spent millions of years hiding in human DNA help the body fight cancer, scientists say.
Researchers at the Francis Crick Institute looked at lung cancer – the leading cause of cancer-related deaths worldwide – to understand why some patients respond better to immunotherapy than others.
They found viral genes passed down by our ancestors can be “woken up” when a person has cancer and join the fight against the tumour.
They hope the discovery could be used to develop a cancer treatment vaccine.
Read more: How cancer vaccines work
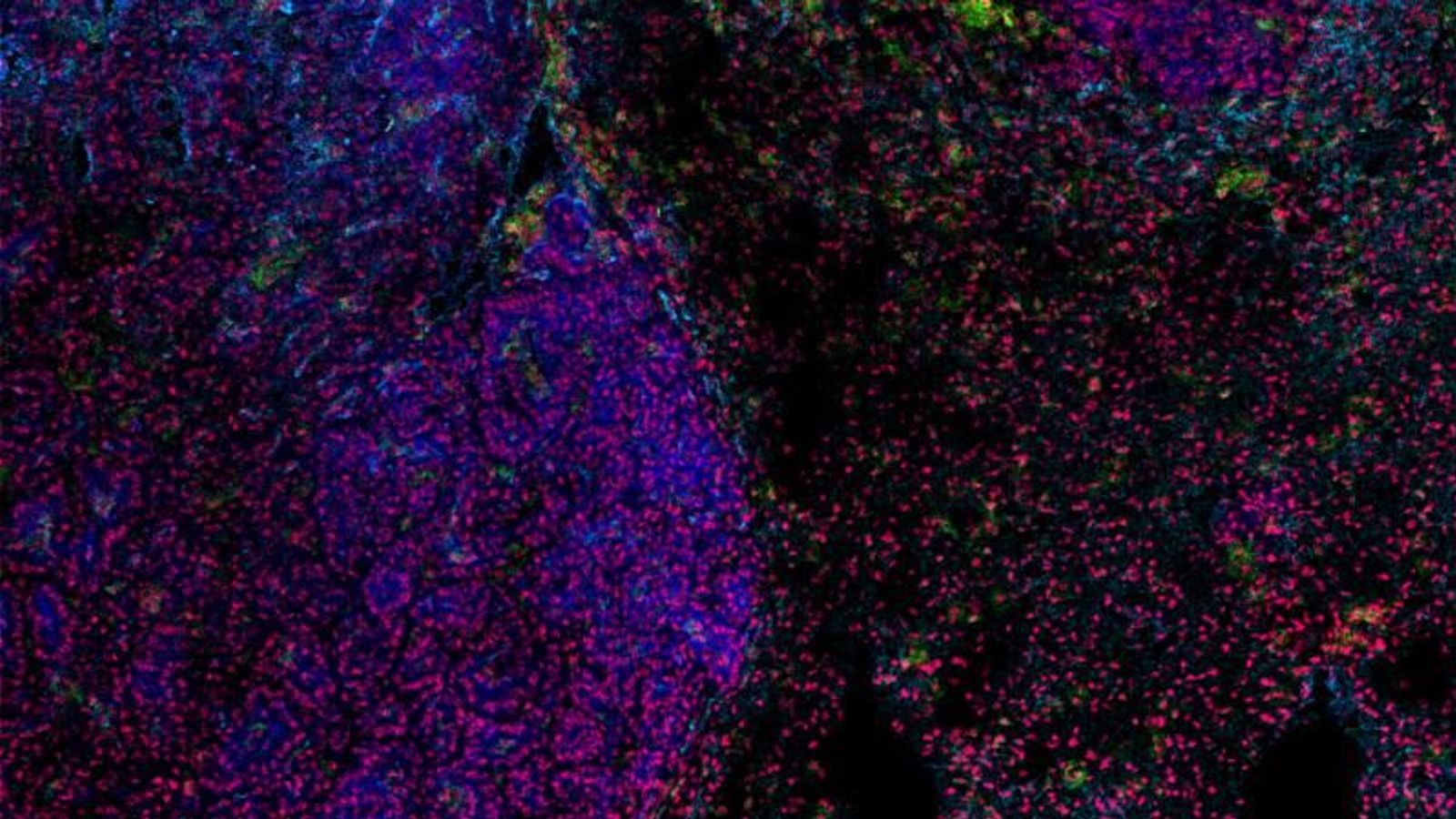
The research team looked at why patients with antibody-producing B cells around their tumour tended to respond better to immunotherapy.
They found these B cells boost the immune response to cancer because they produce antibodies that bind to the tumour.
This is similar to how B cells produce anti-viral antibodies after a flu or COVID infection.
The key to this response is hidden in ancient viral DNA, called endogenous retroviruses (ERVs).
This viral DNA has been passed down from the historic infections of our ancestors and makes up about 5% of human DNA.
It normally lies dormant, but when a person has cancer, the viral genes can be woken up.
The fragments of viruses are enough to trigger an immune response. The body thinks the tumour cells are infected and so attacks them.
Please use Chrome browser for a more accessible video player
Be the first to get Breaking News
Install the Sky News app for free
The research, published in the journal Nature, looked at immune cell activity in mice with lung cancer as well as tumour samples from people with lung cancer. It is part of the TRACERx study, funded by Cancer Research UK.
George Kassiotis, head of the Retroviral Immunology Laboratory at the Crick, said: “ERVs have been hiding as viral footprints in the human genome for thousands or millions of years, so it’s fascinating to think that the diseases of our ancestors might be key to treating diseases today.
“With more research, we could look to develop a cancer treatment vaccine made up of activated ERV genes to boost antibody production at the site of patient’s cancer and hopefully improve the outcome of immunotherapy treatment.”